At the start of the new year, WiRED International’s community health workers (CHWs) in Kenya picked up their active schedule of community health assistance. They live and operate in Kisumu, where they focus their work in the six informal settlements (slums). Thousands of people who live in these settlements face poverty, unemployment and food scarcity every day.
 Until the WiRED CHW team began its work during the COVID-19 pandemic, people in the settlements had few health resources — much less health advocates — to care for their health needs amid the pandemic and developing infectious and noncommunicable diseases.
Until the WiRED CHW team began its work during the COVID-19 pandemic, people in the settlements had few health resources — much less health advocates — to care for their health needs amid the pandemic and developing infectious and noncommunicable diseases.
WiRED’s CHWs in Kisumu record the number of people reached in clinical and instructional settings and the health issues people in these communities face every month. We report the numbers later in this story. But statistics, while important, can never match the power and immediacy of personal stories.
 The following CHWs’ reports bring their work to life and demonstrate their increasing value to the community — a service which will face challenges if, as some media report, there are shortages of vaccines and medical supplies due to delayed or discontinued humanitarian aid.
The following CHWs’ reports bring their work to life and demonstrate their increasing value to the community — a service which will face challenges if, as some media report, there are shortages of vaccines and medical supplies due to delayed or discontinued humanitarian aid.
These four first-person accounts describe typical interventions provided daily by the CHW teams deployed to the informal settlements.
Persistence Pays Off for an HIV/AIDS Patient

 In one of the previous months during my fieldwork in my community I came across a woman with HIV/AIDS who was in denial about having the disease. I talked to her about the benefits of taking antiviral drugs, but my efforts yielded no seed. I continued talking to her for three weeks, and eventually she gave in but confirmed to me that she would not take the drugs in any of the nearest hospitals, I think because of fear of being labeled with HIV/AIDS. We talked more, and she agreed to go to a hospital away from her area. I personally took the risk of taking the woman to the hospital of her choice for HIV/AIDS treatment. I continue to follow up with her and currently she is taking her drugs regularly.
In one of the previous months during my fieldwork in my community I came across a woman with HIV/AIDS who was in denial about having the disease. I talked to her about the benefits of taking antiviral drugs, but my efforts yielded no seed. I continued talking to her for three weeks, and eventually she gave in but confirmed to me that she would not take the drugs in any of the nearest hospitals, I think because of fear of being labeled with HIV/AIDS. We talked more, and she agreed to go to a hospital away from her area. I personally took the risk of taking the woman to the hospital of her choice for HIV/AIDS treatment. I continue to follow up with her and currently she is taking her drugs regularly.
— Mary Atieno, CHW
Changing Cultural Perceptions about Nosebleed

 In Africa, particularly my Luo tribe, many people associate nosebleed with some incorrect cultural perceptions. It is sometimes very hard to tell those who believe in such myths that nosebleed (epistaxis) is connected with medical conditions. Nosebleed can be caused by environmental factors and medical conditions resulting from accidents, dry air, high blood pressure and sinus infections. During my field work engagement sensitizing the members of the community during a health class, I was able to perform first aid for one of the boys who fell down at a sporting activity and got a nosebleed.
In Africa, particularly my Luo tribe, many people associate nosebleed with some incorrect cultural perceptions. It is sometimes very hard to tell those who believe in such myths that nosebleed (epistaxis) is connected with medical conditions. Nosebleed can be caused by environmental factors and medical conditions resulting from accidents, dry air, high blood pressure and sinus infections. During my field work engagement sensitizing the members of the community during a health class, I was able to perform first aid for one of the boys who fell down at a sporting activity and got a nosebleed.
Having received WiRED basic training in first aid, it was very easy to manage the nose bleed. Thereafter I continued with my session to educate the group about the management, environmental and medical explanations about nosebleed. After this engagement, the participants understood very well that nosebleed can be caused by environmental and medical conditions other than cultural perceptions.
— Daniel Ayieko, CHW
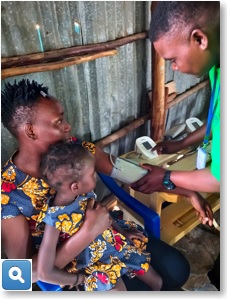
Immunization Rates Up in Kisumu Community

 Immunization status among our community is much improved because people are getting enough information on the value of vaccines and keeping to their dosage schedules. As CHWs we stress the importance of immunizations received at birth, after six weeks, after 10 weeks, after 14 weeks and beyond. I advise young parents to take their children to the health centers every month for five years. The information that parents receive from WiRED CHWs makes the numbers of immunizations defaulters to decrease in the community as a whole — hence children are growing well. Through WiRED I am so gratified to work with community residents to get the health information that they were not aware of and the help that they need.
Immunization status among our community is much improved because people are getting enough information on the value of vaccines and keeping to their dosage schedules. As CHWs we stress the importance of immunizations received at birth, after six weeks, after 10 weeks, after 14 weeks and beyond. I advise young parents to take their children to the health centers every month for five years. The information that parents receive from WiRED CHWs makes the numbers of immunizations defaulters to decrease in the community as a whole — hence children are growing well. Through WiRED I am so gratified to work with community residents to get the health information that they were not aware of and the help that they need.
— Carren Osomo, CHW
Syphilis Case, Referral and Follow-Up

 In the years I have worked as a WiRED CHW I have referred many cases to medical professionals. One particular referral I made stayed in my mind. This was a case of syphilis, which involved a beautiful lady who did not know what was happening to her body until I took her to a clinic. There she was diagnosed with this disease and agreed to take medication, I followed up with the doctor until right now when the woman has finished her treatment. She is doing fine and she agreed to take on preventive measures such as using condoms and many others.
In the years I have worked as a WiRED CHW I have referred many cases to medical professionals. One particular referral I made stayed in my mind. This was a case of syphilis, which involved a beautiful lady who did not know what was happening to her body until I took her to a clinic. There she was diagnosed with this disease and agreed to take medication, I followed up with the doctor until right now when the woman has finished her treatment. She is doing fine and she agreed to take on preventive measures such as using condoms and many others.
— Bunnyce Atieno, CHW
CHW Statistics for January
During the month of January 2025, 20 CHWs in Kisumu, Kenya, reached a total of 8,402 people with health services. Working 24 hours per week, each of the CHWs met with at least 24 patients a week, and the largest number seen in a week by a single CHW was 262, most of them in health training classes.
 This January the top health-related issues recorded by CHWs were as follows in order of prevalence:
This January the top health-related issues recorded by CHWs were as follows in order of prevalence:
-
- Malaria
- Mental health
- HIV/AIDS
- Tuberculous
- Cholera
- Family planning
- Nutrition


