By Allison Kozicharow; Edited by Elizabeth Fine
 In August WiRED International community health workers (CHWs) in Kisumu, Kenya continued to address local mpox concerns while preventing and spotting endemic diseases such as cholera, malaria and HIV/AIDS.
In August WiRED International community health workers (CHWs) in Kisumu, Kenya continued to address local mpox concerns while preventing and spotting endemic diseases such as cholera, malaria and HIV/AIDS.
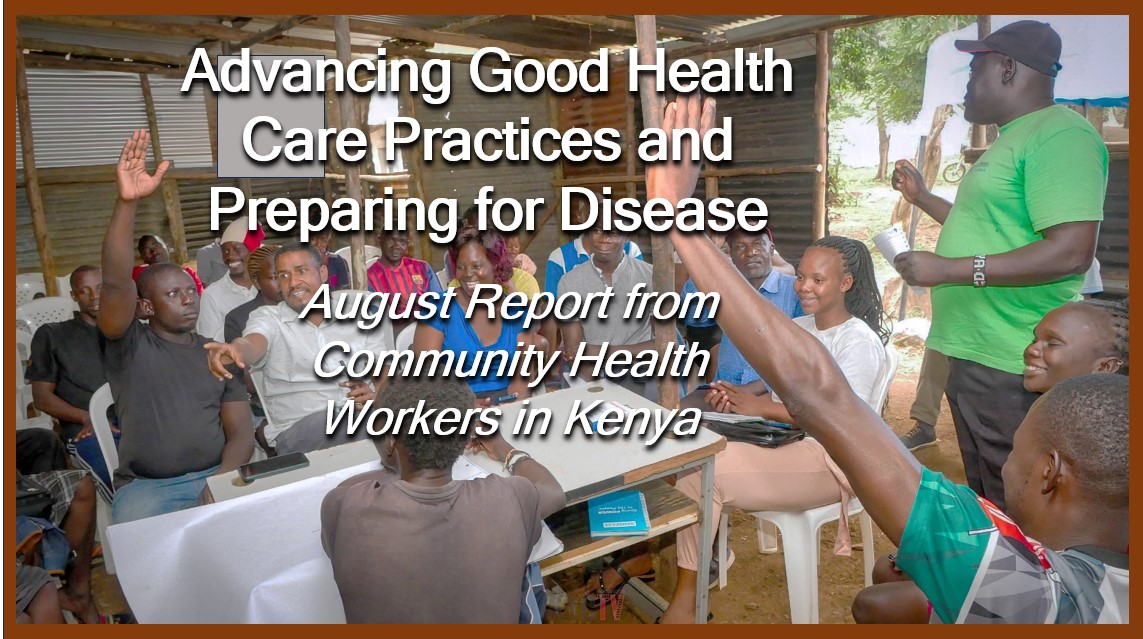
 Mpox is a new worry among Kenyan populations. In an article in mid-August WiRED reported on a special training session held for CHWs in Kisumu. Led by a clinician, the CHWs studied our Mpox module in preparation for a possible mpox outbreak. The following stories illustrate how educating themselves first on a disease enables CHWs to teach their communities how to recognize symptoms, avoid disease transmission and seek appropriate treatment.
Mpox is a new worry among Kenyan populations. In an article in mid-August WiRED reported on a special training session held for CHWs in Kisumu. Led by a clinician, the CHWs studied our Mpox module in preparation for a possible mpox outbreak. The following stories illustrate how educating themselves first on a disease enables CHWs to teach their communities how to recognize symptoms, avoid disease transmission and seek appropriate treatment.
This month I learned about the viral disease mpox. In the past I believed that mpox and scabies were one disease until I studied the WiRED Mpox module through their website portal. I learned that mpox is a zoonotic virus, which is transmitted from animals to humans, with rodents and primates the primary carriers. This knowledge has helped me in my field work because I can respond and teach my community on mpox, including symptoms such as fever, headache, muscle aches and the progression of macules to papules to vesicles to pustules to scabs.

—CHW Daniel Atieno
 At the end of August I began educating members of my community about the deadly mpox virus. Mpox has been confirmed in Kenya with different cases in different towns. I explained to people that the virus can spread from person to person through close contact with respiratory secretions [coughs, sneezes, talking, laughing] and through skin lesions. My information caught people unaware because they thought mpox came only from monkeys. I explained transmission from animals to humans and then humans to humans.
At the end of August I began educating members of my community about the deadly mpox virus. Mpox has been confirmed in Kenya with different cases in different towns. I explained to people that the virus can spread from person to person through close contact with respiratory secretions [coughs, sneezes, talking, laughing] and through skin lesions. My information caught people unaware because they thought mpox came only from monkeys. I explained transmission from animals to humans and then humans to humans.
 I also educated them on prevention measures such as washing hands well with soap and water after any contact with an infected person or animal. I encouraged them to use an alcohol-based hand sanitizer if soap and water were not available. I advised people to always report to the nearest health facility for isolation and treatment in case of their developing any of the symptoms we discussed, especially any skin lesions.
I also educated them on prevention measures such as washing hands well with soap and water after any contact with an infected person or animal. I encouraged them to use an alcohol-based hand sanitizer if soap and water were not available. I advised people to always report to the nearest health facility for isolation and treatment in case of their developing any of the symptoms we discussed, especially any skin lesions.
—CHW Linet Awuor
 The CHW stories demonstrate the need for CHWs — trained and part of their communities — to provide ongoing health care, diagnosis, treatment and surveillance and to make referrals to medical facilities when appropriate. Of note, the CHWs keep learning through WiRED’s required Continuing Medical Education requirements and through studying new modules WiRED creates when outbreaks such as mpox occur. In low-resource areas of the world where doctors and adequate health systems are limited, CHWs not only fill that gap but bridge it.
The CHW stories demonstrate the need for CHWs — trained and part of their communities — to provide ongoing health care, diagnosis, treatment and surveillance and to make referrals to medical facilities when appropriate. Of note, the CHWs keep learning through WiRED’s required Continuing Medical Education requirements and through studying new modules WiRED creates when outbreaks such as mpox occur. In low-resource areas of the world where doctors and adequate health systems are limited, CHWs not only fill that gap but bridge it.

CHW Statistics for August 2024
During the month of August 2024, 19 CHWs in Kisumu, Kenya, reached a total of 8,495 people with health services. Working 24 hours per week, each of the CHWs met with at least 65 patients a week, and the largest number seen in a week by a single CHW was 175, most of them in health training classes.
In August, the top health-related concerns were, as follows, in order of prevalence:
-
 Mpox
Mpox- Cholera
- Malaria
- HIV/AIDS
- Menstrual health
- Typhoid
- Infectious diseases