By Allison Kozicharow; Edited by Elizabeth Fine
In recent months, health challenges have escalated dramatically in the world’s poorest regions. U.S. government cutbacks have reduced access to medicines and vaccines and forced thousands of health workers out of their jobs. Already struggling with a critical shortage of doctors, these regions now face new unprecedented health threats.
 Can Community Health Workers (CHWs) help alleviate the burden on the medical community? Is it possible to equip these health workers with the necessary skills to address the growing gaps in care, and can even the smallest communities afford to train CHW teams?
Can Community Health Workers (CHWs) help alleviate the burden on the medical community? Is it possible to equip these health workers with the necessary skills to address the growing gaps in care, and can even the smallest communities afford to train CHW teams?
WiRED International answers these questions in a journal article entitled “Community Health Workers: A Narrative Review of a Curriculum and Training Program for Low-Income Communities Facing Limited Access to Healthcare,” just published in the journal Frontiers in Public Health.
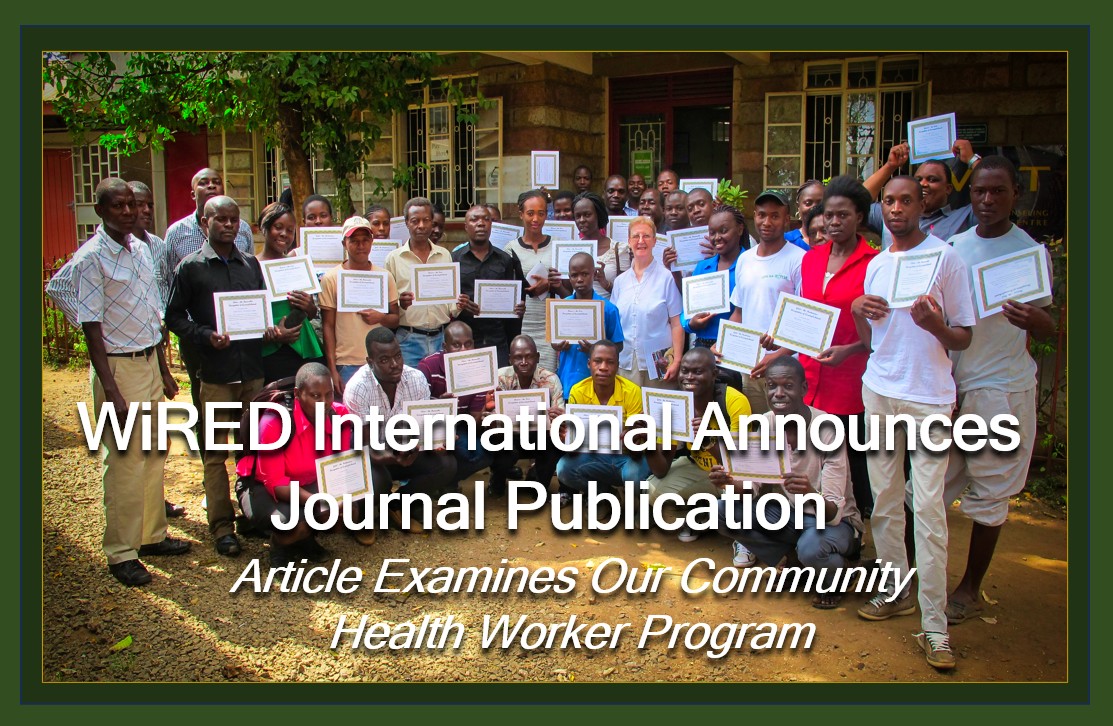
 The paper was co-written by WiRED International Medical Programs Director Maryam Othman, M.D., M.P.H., and WiRED Executive Director Gary Selnow, Ph.D. Drs. Othman and Selnow examined WiRED’s CHW training program and assessed its impact through a case study of WiRED’s 20-member CHW team in Kisumu, Kenya. The authors’ goal was to describe the curriculum and offer the program for easy access in other underserved communities around the world.
The paper was co-written by WiRED International Medical Programs Director Maryam Othman, M.D., M.P.H., and WiRED Executive Director Gary Selnow, Ph.D. Drs. Othman and Selnow examined WiRED’s CHW training program and assessed its impact through a case study of WiRED’s 20-member CHW team in Kisumu, Kenya. The authors’ goal was to describe the curriculum and offer the program for easy access in other underserved communities around the world.
The authors reported that WiRED adopted the following principles as mandatory for the CHW training program:
 WHO-compliancy
WHO-compliancy- Professionally produced, evidence-based and peer-reviewed training material
- A curriculum with interactive training modules and quizzes
- A library of health modules available online and for downloading onto smart phones and tablets
- Active learning through classroom instruction, ongoing student collaborations
- A curriculum relevant to populations globally but adaptable to local needs per WHO urging
- In-person classes taught by medical professionals from the same area to be served by the CHWs
- Final examination and certification by WiRED
- A continuing medical education (CME) requirement — vital to maintain and grow skills
- All materials and services provided to be offered cost-free
 Drs. Othman and Selnow summarized the WiRED CHW curriculum. Thirty-four modules comprised four training blocks: Core Health, Clinical Issues, First Aid and Critical Care and Communication (including teaching methods and health surveillance strategies). The authors described the distribution of the WiRED program, which capitalizes on the growing use of smartphones and provides a phone app to the entire library of health training modules.
Drs. Othman and Selnow summarized the WiRED CHW curriculum. Thirty-four modules comprised four training blocks: Core Health, Clinical Issues, First Aid and Critical Care and Communication (including teaching methods and health surveillance strategies). The authors described the distribution of the WiRED program, which capitalizes on the growing use of smartphones and provides a phone app to the entire library of health training modules.
 Drs. Othman and Selnow looked at the Kisumu team’s results. The 20 WiRED CHWs reach more than 9,000 people each month with clinical services, health follow-ups and public health training sessions. In addition to the reported monthly activity and outcome reports, CHWs are invited to write brief narratives describing the people they encounter and the health services they provide in their community. These accounts are collected, transcribed and cataloged as anecdotal evidence of the work CHWs accomplish on a routine basis. Sample narratives cover health-screening clinics, teaching about emerging diseases, preventing cholera through proper water treatment and assisting HIV/AIDS victims.
Drs. Othman and Selnow looked at the Kisumu team’s results. The 20 WiRED CHWs reach more than 9,000 people each month with clinical services, health follow-ups and public health training sessions. In addition to the reported monthly activity and outcome reports, CHWs are invited to write brief narratives describing the people they encounter and the health services they provide in their community. These accounts are collected, transcribed and cataloged as anecdotal evidence of the work CHWs accomplish on a routine basis. Sample narratives cover health-screening clinics, teaching about emerging diseases, preventing cholera through proper water treatment and assisting HIV/AIDS victims.
 Drs. Othman and Selnow concluded that the WiRED CHW training program offers many solutions to the health crises faced now by underserved communities worldwide and in the future as the shortage of medicines and vaccines begins to ravage populations in poor countries.
Drs. Othman and Selnow concluded that the WiRED CHW training program offers many solutions to the health crises faced now by underserved communities worldwide and in the future as the shortage of medicines and vaccines begins to ravage populations in poor countries.
[The program] avoids most financial hurdles; it encourages local adoption and implementation without involving large bureaucratic institutions or lengthy application procedures. The evidence-based, professional curriculum properly prepares CHWs, and several provisions render the training relevant to local conditions. Finally, the all-important CME component, supported by non-profit sponsors, ensures that the CHWs continue their development as community health needs and conditions change over time.
About the Frontiers in Public Health Journal
Frontiers in Public Health was founded in 2007 by Henry Markram and Kamila Markram, neuroscientists from the Swiss federal Institute of Technology in Lausanne, Switzerland. Starting from neuroscience, the journal today “spans hundreds of academic disciplines and is one of the most cited and largest research publishers in the world.” The journal’s mission “is to make science open so that scientists can collaborate better and innovate faster to deliver the solutions that enable healthy lives on a healthy planet.”
The Authors
Dr. Maryam Othman is WiRED’s Director of Medical Education, bringing a wealth of medical and international public health experience. She manages all content for WiRED’s Community Health Training Program and develops the texts for the tutorials and study materials. Currently, Dr. Othman is Chief of Global Health Section in the Department of Population Health Science and Assistant Professor at Western University of Health Science College of Osteopathic Medicine. She received her M.D. from the University of Baghdad, Iraq, and her M.P.H. in global health management from The George Washington University, where she was a Fulbright Scholar. She was the Senior National Medical Officer of the International Organization for Migration Baghdad, Iraq, from July 2003 to January 2006.
Dr. Gary Selnow is WiRED’s Founder and Executive Director. He is Professor Emeritus at San Francisco State University and the author/co-author of seven books. Dr. Selnow was twice a Fulbright Scholar and served on a White House task force. He was a regular commentator on NPR’s Marketplace program and a consultant for NBC television and the National Academy of Sciences. He was awarded the 2004 President’s Medal at San Francisco State University and the UC Berkeley Public Health Award.
The authors offered the following comments about their article and the value of CHWs:
From Dr. Othman
As someone who was medically trained in a low-resource country, I fully understand the challenges facing our CHWs. Unfortunately, their routine challenges are made much worse by recent government cutbacks in international health. I believe that the WiRED CHW training program fully prepares CHWs to overcome many of the problems now becoming evident with the absence of medicines and vaccines. Local CHWs know the region and the people, and they can be highly creative in identifying solutions. Moreover, they can scale up their outreach efforts and expand their work to nearby communities with cooperative, neighbor-to-neighbor health programs.
From Dr. Selnow
Every community, no matter how small, would welcome having a local doctor on call. However, given the scarcity of doctors in low-resource environments, this is unlikely to become a reality — and the situation is expected to worsen in the years ahead. I have seen firsthand how well-trained CHWs can step in to fill this gap. They can provide essential clinical services, teach prevention, and serve as an active bridge to medical professionals.
Recognizing the potential of CHWs, WiRED developed a rigorous program featuring six weeks of training and an ongoing continuing medical education component. This program equips local CHWs to serve where doctors are scarce; to help the ailing, to educate the vulnerable, to take the sickest patients for higher-level care. WiRED’s training program stands as a testament to the reality that CHWs can elevate health care in isolated and underserved communities. The WIRED CHW training program is not a business, because it is free; it is not a hunch, because it is proven; and it is not just a promise, because it is available now to any community ready to prepare a CHW team.